Keratoconus: Understanding Corneal Deformation and Treatments in Geneva
Focus Keyphrase: Keratoconus Geneva
SEO Title (English): Keratoconus Geneva: Symptoms, Causes & Innovative Treatments
SEO Description (English): Learn about keratoconus in Geneva, a corneal deformation. Discover the symptoms, possible causes, and available treatments, from contact lenses to surgery. Expert ophthalmology practice in Geneva.
What is Keratoconus? The Cone-Shaped Cornea: Simple Explanation
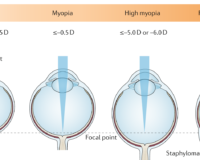
Keratoconus is an eye condition that affects the cornea, the clear, dome-shaped front surface of your eye, like the watch crystal of a watch. In keratoconus, the cornea, instead of maintaining its normal rounded shape, gradually thins and bulges outward into a cone shape. Imagine a tent where one of the poles collapses: the canvas would deform and take on a conical shape.
Keratoconus is a progressive disease that usually begins in adolescence or early adulthood and slowly progresses over several years, before stabilizing in most cases. It affects both eyes, but often asymmetrically (one eye may be more affected than the other).
Symptoms of Keratoconus: How to Recognize It?
Symptoms of keratoconus appear gradually and vary depending on the stage of the disease. The most common signs include:
- Blurred and distorted vision: Even with glasses, vision may remain blurry. Straight lines may appear wavy or distorted.
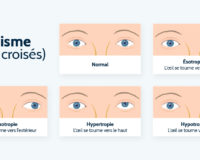
- Irregular astigmatism: Astigmatism is a defect in the curvature of the cornea. In keratoconus, astigmatism becomes irregular and difficult to correct with conventional glasses.
- Increased sensitivity to light (photophobia) and glare.
- Double vision (diplopia), sometimes even with one eye open.
- Frequent changes in eyeglass prescriptions: Needing to change glasses more and more often, without significant improvement in vision.
- Difficulty seeing at night.
- Eye strain, eye fatigue.
It is important to consult an ophthalmologist if you experience these symptoms, as they may indicate keratoconus, but also other eye problems. Early diagnosis is essential for appropriate management.
Causes of Keratoconus: Why Does the Cornea Deform?
The exact causes of keratoconus are not yet fully understood, but a combination of genetic and environmental factors appears to be involved:
- Genetic factor: Keratoconus is more common in people with a family history of the disease. Several predisposing genes have been identified, but the inheritance pattern is complex.
- Environmental factors:
- Repeated eye rubbing: Rubbing your eyes excessively and vigorously is considered a significant and modifiable risk factor.
- Eye allergies (allergic conjunctivitis): Chronic eye allergies, which encourage eye rubbing, may promote keratoconus.
- Wearing ill-fitting contact lenses.
- Certain systemic diseases: Associations have been observed with certain conditions such as Down syndrome, Ehlers-Danlos syndrome, or osteogenesis imperfecta.
Although the precise causes remain to be determined, it is important to remember that excessive eye rubbing is a modifiable risk factor that can be addressed.
Diagnosis of Keratoconus: Decisive Eye Examinations
Keratoconus is diagnosed by an ophthalmologist during a comprehensive eye exam. Key examinations include:
- Visual acuity measurement and refraction: To assess the quality of vision with and without optical correction (glasses). Refraction may reveal irregular astigmatism.
- Corneal topography: This is the most important examination for diagnosing and monitoring keratoconus. A corneal topographer is a device that analyzes the curvature of the cornea at many points and maps its shape in relief. It allows visualization of the characteristic conical deformation of keratoconus, even at an early stage.
- Corneal pachymetry: Measurement of corneal thickness. In keratoconus, the cornea is usually thinned, especially in the conical area.
- Slit-lamp examination: Microscope used to examine the cornea in detail and visualize specific signs of keratoconus (Vogt's striae, Fleischer ring, etc.).
- Retinoscopy: Technique to assess eye refraction and detect irregular astigmatism.
These examinations are painless and allow the ophthalmologist to confirm the diagnosis of keratoconus, assess its stage of severity, and monitor its progression.
Treatments for Keratoconus: Solutions Adapted to Each Stage
There is no cure for keratoconus, but effective treatments are available to improve vision and stop or slow disease progression. Keratoconus management is progressive and adapted to the stage of the disease:
Initial and Mild Stage: Glasses and Soft Contact Lenses
- Glasses: In early keratoconus, glasses may be sufficient to correct astigmatism and improve vision.
- Toric soft contact lenses: If glasses are no longer sufficient, toric soft lenses specifically for astigmatism can provide better vision.
Moderate to Advanced Stage: Special Lenses and Intracorneal Rings
- Rigid gas permeable (RGP) contact lenses: These lenses are more uncomfortable at first, but they offer better vision than soft lenses in keratoconus. They regularize the corneal surface and compensate for irregularity.
- Hybrid lenses: Combine a rigid central part for good vision and a soft periphery for comfort.
- Scleral or mini-scleral lenses: Large rigid lenses that rest on the sclera (the white of the eye) and not on the cornea. They are often well tolerated and provide excellent vision, even in advanced keratoconus.
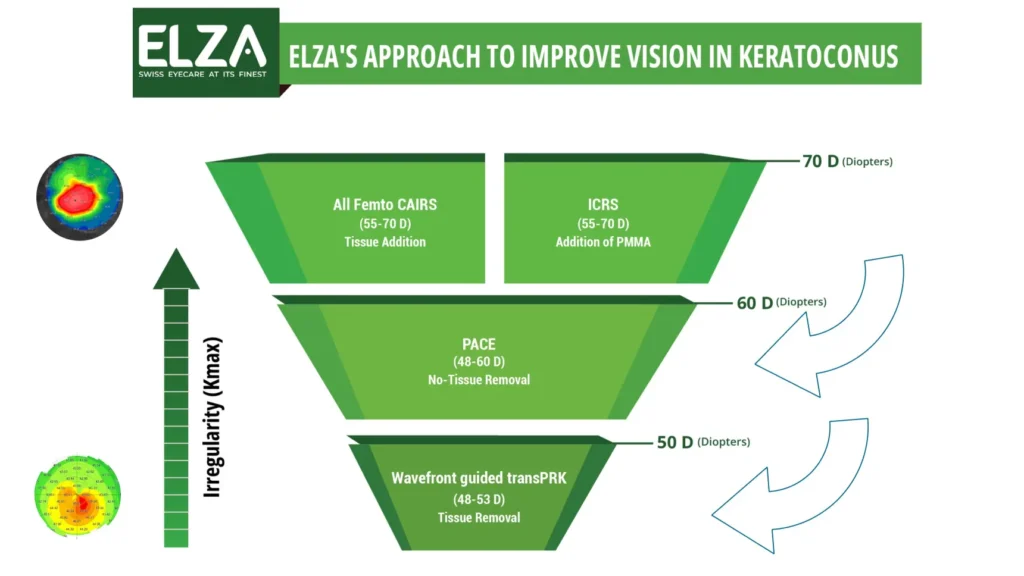
- Intracorneal ring segments (intacs): Segments of biocompatible plastic rings inserted into the corneal stroma to reshape its form and reduce conical deformation. They can improve vision and facilitate contact lens wear.
- Corneal cross-linking (CXL): Treatment aimed at strengthening the cornea and stopping or slowing the progression of keratoconus. It involves applying riboflavin (vitamin B2) to the cornea and then exposing it to UV-A light. Cross-linking is often offered as soon as progressive keratoconus is diagnosed.
Very Advanced Stage: Corneal Transplant (Keratoplasty)
- Corneal transplant (keratoplasty): As a last resort, in very advanced keratoconus where other treatments are no longer sufficient to ensure functional vision, a corneal transplant may be considered. It involves replacing the central part of the diseased cornea with a healthy cornea from a donor. Different corneal transplant techniques exist (penetrating keratoplasty, deep anterior lamellar keratoplasty, DMEK, DSAEK).
The choice of the most appropriate treatment will depend on the stage and severity of keratoconus, your vision, your contact lens tolerance, and your personal needs. Regular follow-up with your ophthalmologist is essential to adjust treatment and monitor progression.
Living with Keratoconus: Tips and Adaptation
Living with keratoconus can be challenging, but it is possible to lead a normal life with appropriate management. Some tips:
- Strictly follow your ophthalmologist's recommendations: Contact lens wear, eye drops, follow-up exams, etc.
- Avoid rubbing your eyes: This is essential to slow the progression of keratoconus. If you have eye allergies, treat them effectively to reduce itching.
- Protect your eyes from the sun: Wear good quality sunglasses, even on cloudy days.
- Be patient and persevering with contact lens wear: Adapting to special lenses for keratoconus can take time, but they are often essential for good vision.
- Don't hesitate to ask for help and support: Talk to your loved ones, join patient support groups for people with keratoconus.
- Use visual aids if necessary: Magnifiers, adapted lighting, etc.
With regular ophthalmological follow-up and appropriate treatments, it is possible to live well with keratoconus and maintain a good quality of life.
Keratoconus and Your Vision in Geneva: Our Specialized Ophthalmology Practice
If you think you may have keratoconus, have been recently diagnosed, or are seeking expertise for the management of your keratoconus in Geneva, our ophthalmology practice is at your disposal. We perform all necessary examinations for the diagnosis of keratoconus and offer a wide range of treatments, from special contact lenses to surgery, including cross-linking and intracorneal rings.
[Your Ophthalmology Practice Name]
[Your Practice Address in Geneva]
[Phone Number]
[Website (if applicable)]
Consult our ophthalmology practice for medical advice on your case. Book your appointment with us over the phone +41 (0) 22 346 26 78 or through our online booking.





Leave a Comment